Frozen placental explants from control and GDM group 20 mg were used for experiments shown in Fig. Protein hormones Steroid hormones 3.
Second the organ is transient growing and developing during.
Endocrinology and physiology of placenta. 7 Zeilen Placenta Endocrine Function - Anatomy Physiology. The Placenta is a hugely important endocrine organ producing many hormones which affect the status of pregnancy and the maternal physiology. Produced towards the end of pregnancy.
Endocrine Functions of the Placenta. Last Updated on Mon 19 Apr 2021 Human Physiology. The placenta secretes both steroid hormones and protein hormones.
The protein hormones include chorionic gonadotropin hCG and chorionic somatomammotropin hCS both of which have actions similar to those of some anterior pituitary hormones table 207. The formation and development of the placenta is one of these critical pregnancy events. This organ plays essential roles during gestation including fetal nourishment support and protection gas exchange and production of several hormones and other mediators.
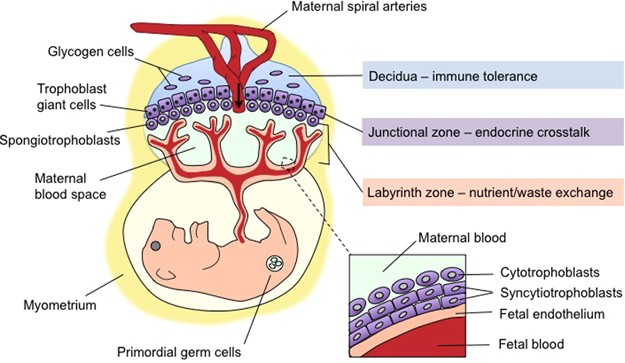
Placental hormones are mainly secreted by the syncytiotrophoblast in a highly and tightly regulated way. These hormones are important for. ENDOCRINOLOGY OF PLACENTA.
The endocrine system a system that is functional from the time of intrauterine existence through old age is one of the first systems to develop during fetal life. Unique to mammals the placenta plays a major role in the growth and development of these fetal systems. Without question the placenta is one of the most.
The maternal component of the placenta varies in different species. The uterus which is developed for retention of the embryo also contributes to the maternal vasculature. Within the placenta maternal and fetal vessels lie in intimate juxtaposition facilitating the exchange of nutrients and waste products.
The endocrine milieu of human pregnancy is dominated by placental hormones the major function of which is to modify maternal physiology to satisfy the nutritional metabolic and physical demands of the growing fetus. In this context the physiologic role of the principal placental hormones is discussed. The placenta is a rather unique endocrine organ.
First since the hormone-producing placental trophoblast cells are derived from the fertilized egg the placenta is genetically distinct from the maternal targets of the placental hormones except of course in matings of highly inbred parents such as inbred strains of mice. Second the organ is transient growing and developing during. Placental endocrinology 1.
At 6-8 weeks there istransfer of functions of corpusluteum to the placenta-whichacts temporarily as a newendocrine organ or powerhouseof hormone production. Protein hormones Steroid hormones 3. The placenta fulfills several critical roles as the interface between mother and fetus.
It prevents rejection of the fetal allograft enables respiratory gas exchange transports nutrients eliminates fetal waste products and secretes peptide and steroid hormones that regulate both maternal metabolism and fetal growth and development. Dehydroepiandrosterone-3-sulfate DHEA-S of maternal and fetal origin contributes about equally to the placental formation of estrone and estradiol whereas 16α-hydroxydehydroepiandrosterone-sulfate 16α-OH-DHEA-S supplied by the fetus contributes to 90 of placental estriol synthesis. This study provides genuine new data into the complex physiology of placental oxygenation in IUGR fetuses.
The higher mitochondrial content in IUGR placental tissue is reversed in cytotrophoblast cells which instead present higher mitochondrial functionality. This suggests different mitochondrial content and activity depending on the placental cell lineage. Increased placental oxygen consumption.
Placental triglyceride determination was determined as described previously. Frozen placental explants from control and GDM group 20 mg were used for experiments shown in Fig. For the rest of the experiments placental explants were preincubated in low or high glucose in the presence of 01 mmoll palmitate for 18 h as described above.
Given that the human placenta is a unique organ having a transient and somewhat defined life span of 280 days any adaption or dysfunction associated with mitochondrial physiology as a result of aging will have a dramatic impact on the health and function of both the placenta and the fetus. Additionally a defective placenta during gestation resulting in reduced fetal growth has been shown. The placenta is a tissue of fetal origin embedded in the maternal uterine wall that permits exchange of vital nutrients and other elements essential for fetal growth development and survival.
In addition the placenta is a tissue capable of steroid and polypeptide synthesis. Hormonal products and interconversions resulting from these synthetic pathways appear to be critically important for ordered. Identifying possible mediators and physiological processes involved in modulating nutrient transport within the placenta is essential to prevent andor develop treatments for the effects of aberrant nutrition nutrient transfer and detrimental changes to fetal development.
A potential role for myostatin as a mediator of nutrient uptake and transport from the mother to the fetus was shown through the recent. Placental glutamate oxidation is likely to serve several functions. Glutamate output by the fetal liver allows the fetus to uncouple the oxidation of glucogenic amino acids from gluconeogenesis.
Glutamate oxidation by placental mitochondria generates NADPH and therefore plays a role in biosynthetic reactions such as steroidogenesis. Endocrine cells in various organs The heart. Atrial natriuretic peptide ANP o Stimulates kidney to secrete more sodium o Thereby decreases excess blood volume high BP and high blood sodium concentration GI tract derivatives.
Diffuse neuroendocrine system DNES The placenta secretes steroid and protein hormones o Estrogens progesterone o CRH o HCG The kidneys o.